Case 1 – 2023
Learning Objectives:
- Recognise the presenting symptoms and clinical signs of Posner Schlossman Syndrome (PSS)
- Formulate a list of differential diagnoses with reasons for exclusion
- Become familiar with the aetiology and epidemiology of PSS
- Describe the management strategies for patients with PSS
- Explain the long-term prognosis for patients with PSS
Case Presentation:
A 42 year-old male presents acutely to your practice with a sore right eye (described as a mild ache). He has noted that over the past day or so the vision in the right eye is more blurred than normal, but he is still able to perform his day-to-day activities. His partner has pointed out that his right eye has looked a bit red and suggested he goes to see his optometrist.
His previous ocular history includes a couple of similar episodes in the past (unsure of timepoints), but he did not see anyone for an assessment at these times because the pain stopped and his vision went back to normal after a few days to a week. He is not sure but thinks that both previous episodes may have also affected his right eye. He has no history of ocular injury or surgery, and has never been prescribed eye drops. He has glasses he wears as needed for distance and near (prescribed overseas) but has not seen an optometrist in over five years.
He reports good general health, and his only current medication is escitalopram for anxiety. He has a family history of wet age-related macular degeneration (mother) but no known history of glaucoma or other eye disease.
Initial examination findings are below:
| Right Eye | Left Eye | |
| Aided distance vision | 6/7.5-2 | 6/4.8 |
| Pinhole visual acuity | No improvement | N/A |
| Refraction | +1.00/-2.00 x 091 | +0.75/-1.25 x 083 |
| Colour Vision (Ishihara Plates) | 14/14 | 14/14 |
| Pupils | No RAPD. RE sluggish response. | |
| IOP (Goldmann at 10:45 am) | 49 mmHg | 16 mmHg |
| Slit-lamp examination | Grade 1 diffuse conjunctival injection. Mild corneal stromal haze, with trace inferior faint white keratic precipitates on corneal endothelium. Van Herick 1.0. Grade 1+ cells in anterior chamber. Vitreous quiet. | Ocular media clear, anterior chamber deep and quiet |
| Corneal Pachymetry | 602 µm | 573 µm |
| Gonioscopy | Open angles (Schafer grade 4 all quadrants), with moderately pigmented trabecular meshwork. No peripheral anterior synechiae. | Open angles (Schafer grade 4 all quadrants), with moderately pigmented trabecular meshwork. |
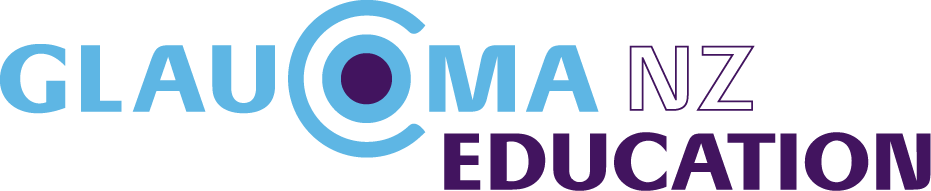
| Fundus examination | See optic nerve photo (Figure 1a). Macula clear. Peripheral retina clear and flat | See optic nerve photo (Figure 1b). Macula clear. Peripheral retina clear and flat |
| Visual Fields | See visual fields (Figures 2a and 2b) | |
| OCT | See RNFL analysis (Figure 3) and GCC scan (Figure 4) | |
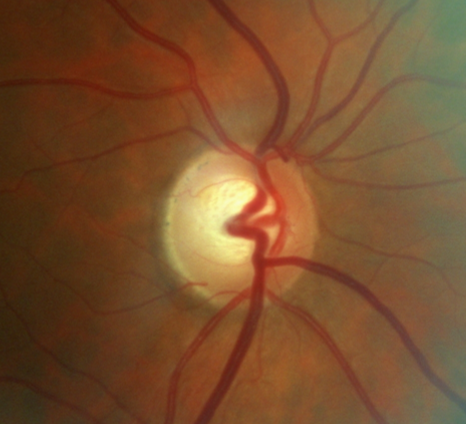
Figure 1 a – R ONH 2015
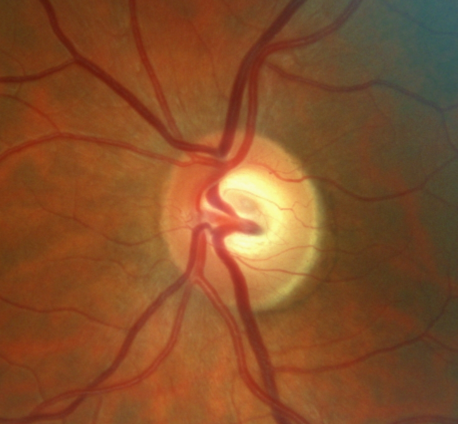
Figure 1 b – L ONH 2015
Figure 2 a – R VF 2015
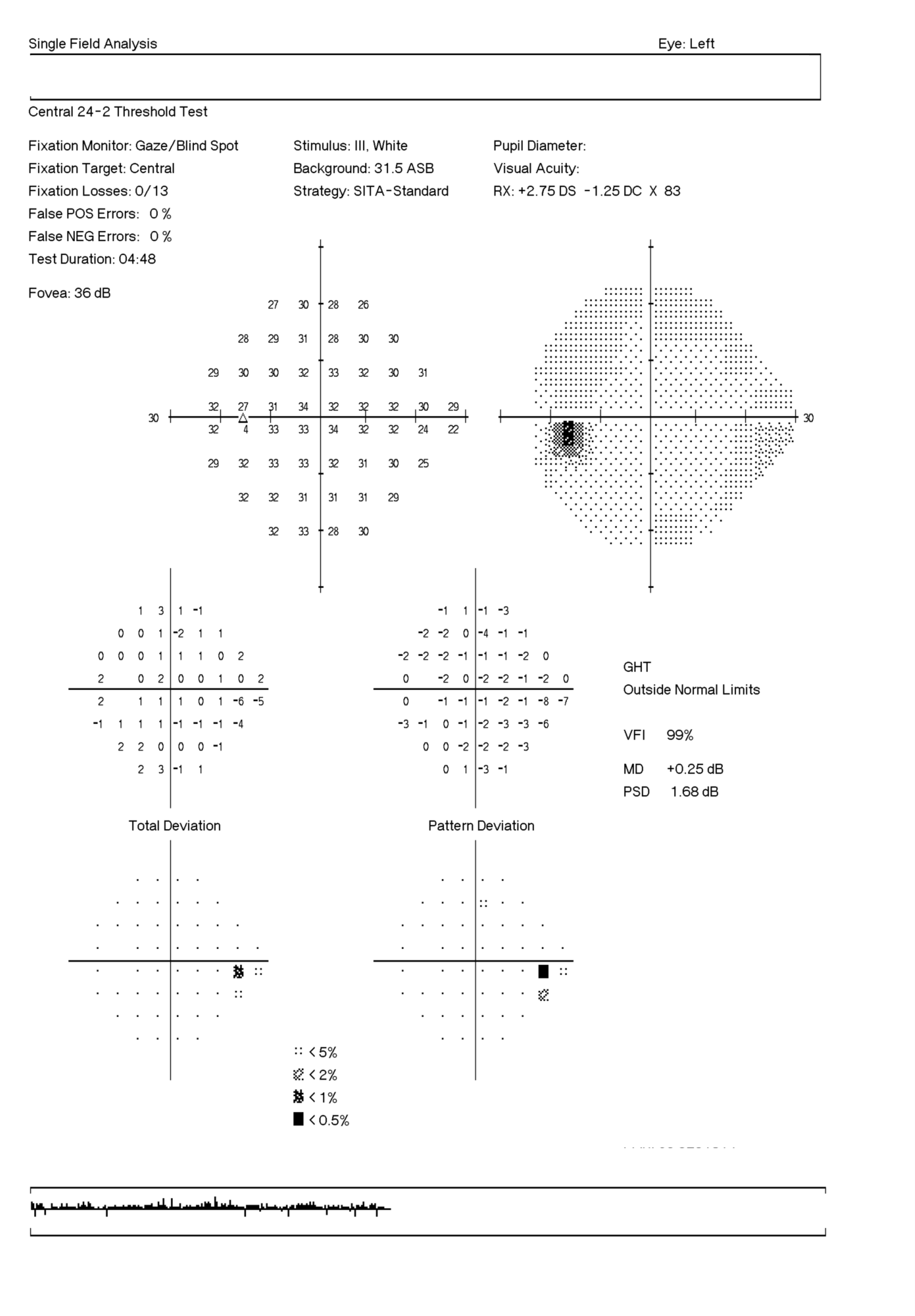
Figure 2 b – L VF 2015
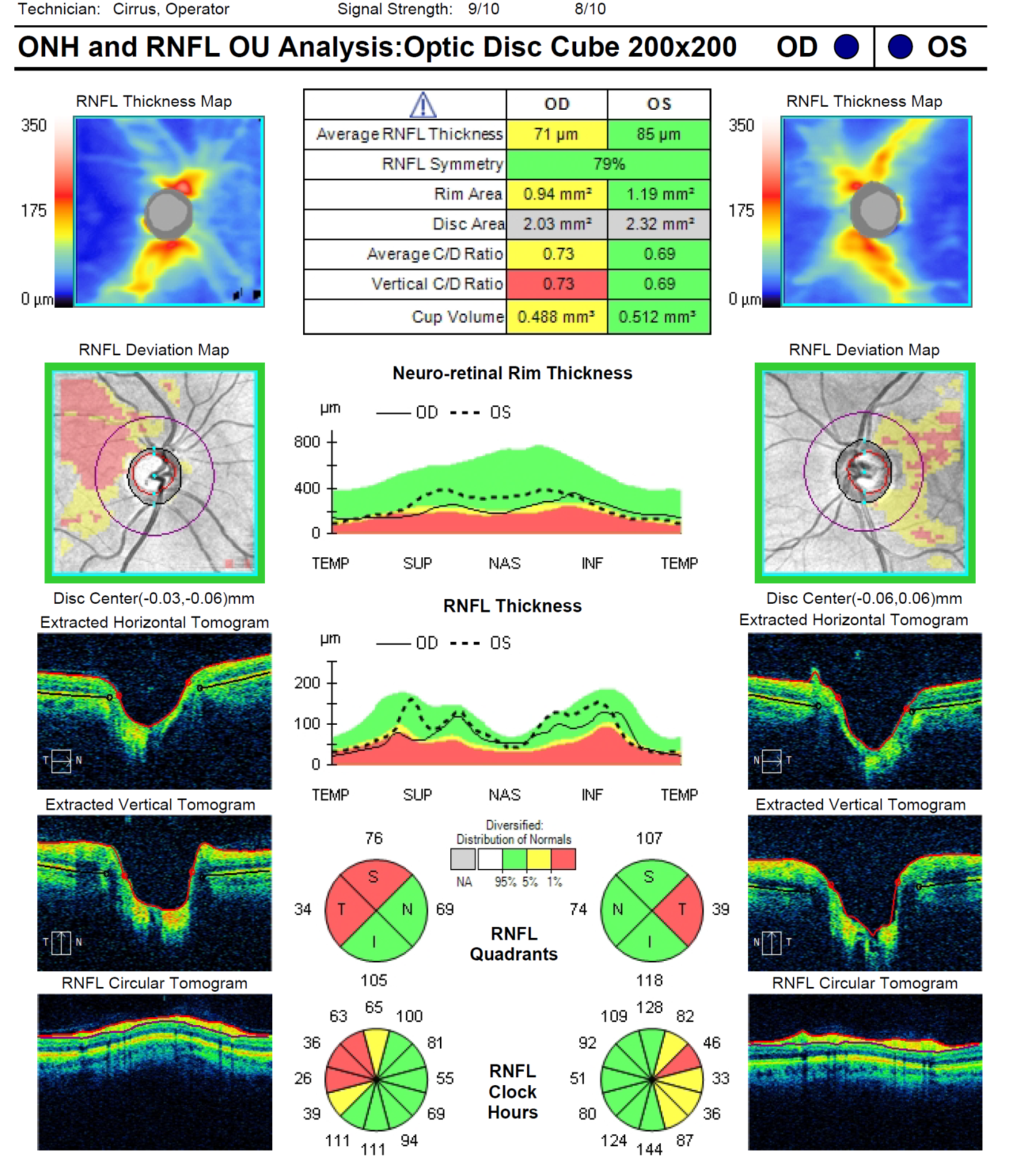
Figure 3 – RNFL OU 2015
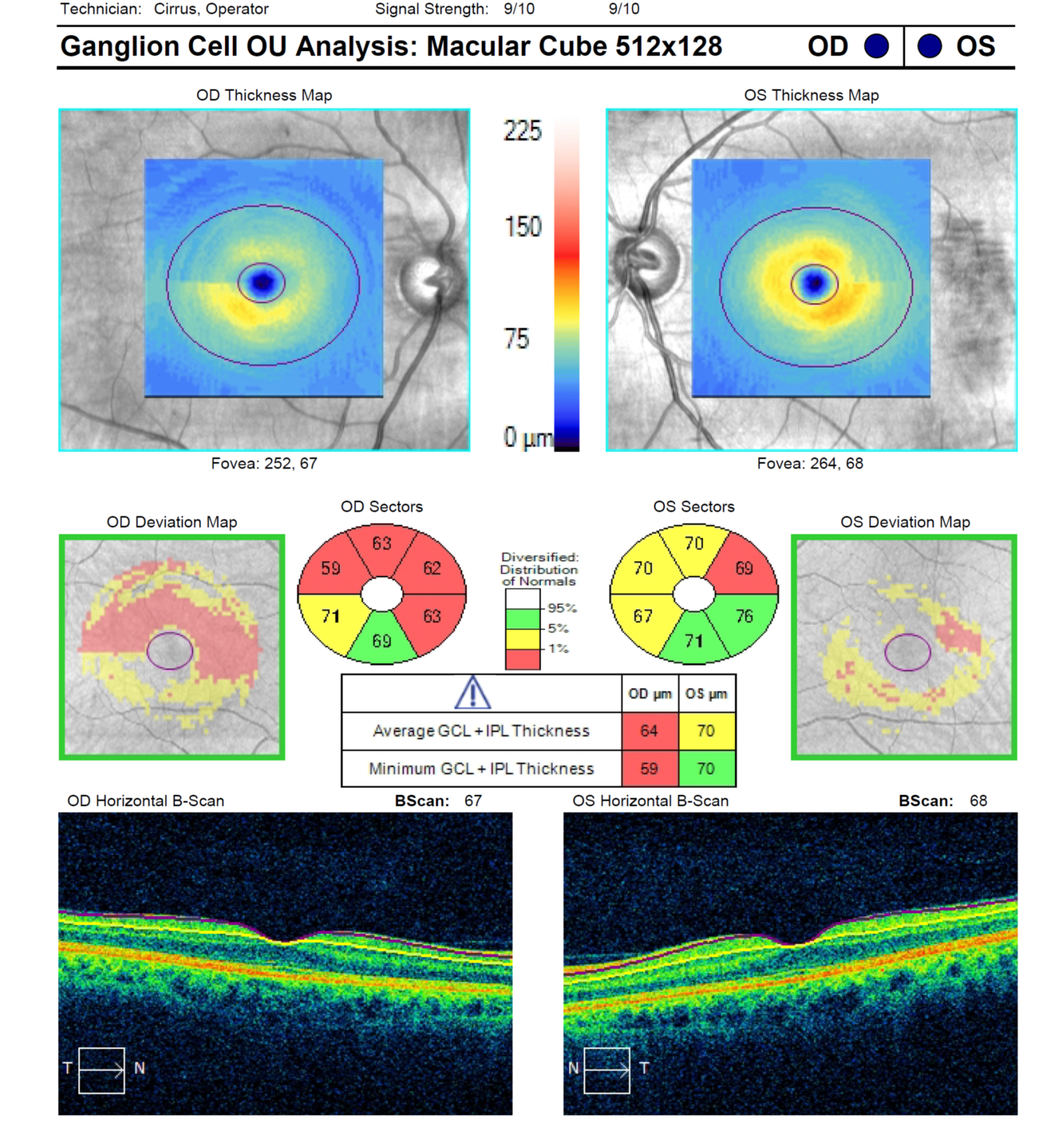
Figure 4 – GCC OU 2015
The patient moves overseas and is lost to follow-up. When he returns to New Zealand three years later, he comes back to see you for another assessment. When asked, he mentions that his adherence to his eye drop routine has been poor and there have been long periods of time that he did not take his ocular medication. He thinks he has had two to three more episodes of PSS during this time, all affecting the right eye. At the time of his visit he is not on any medication, but his eyes feel comfortable and his vision is 6/4.8 in each eye with glasses. His IOP is 21 mmHg in the RE and 14 mmHg in the left.
Please review his optic disc photos (Figures 5a and 5b), visual fields (Figures 6a and 6b), RNFL OCT (Figure 7) and GCC OCT (Figure 8).
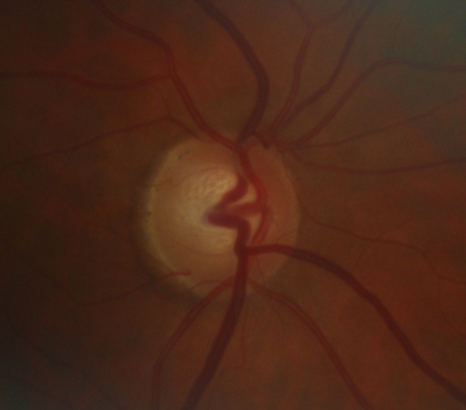
Figure 5 a- R ONH 2022
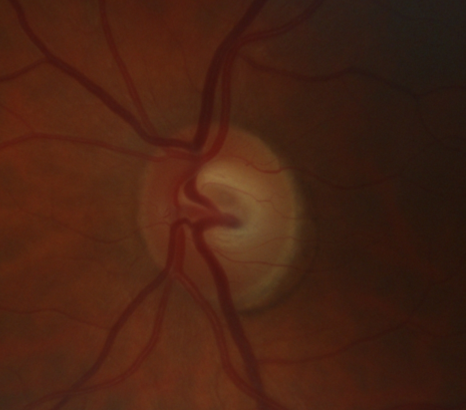
Figure 5 b – L ONH 2022
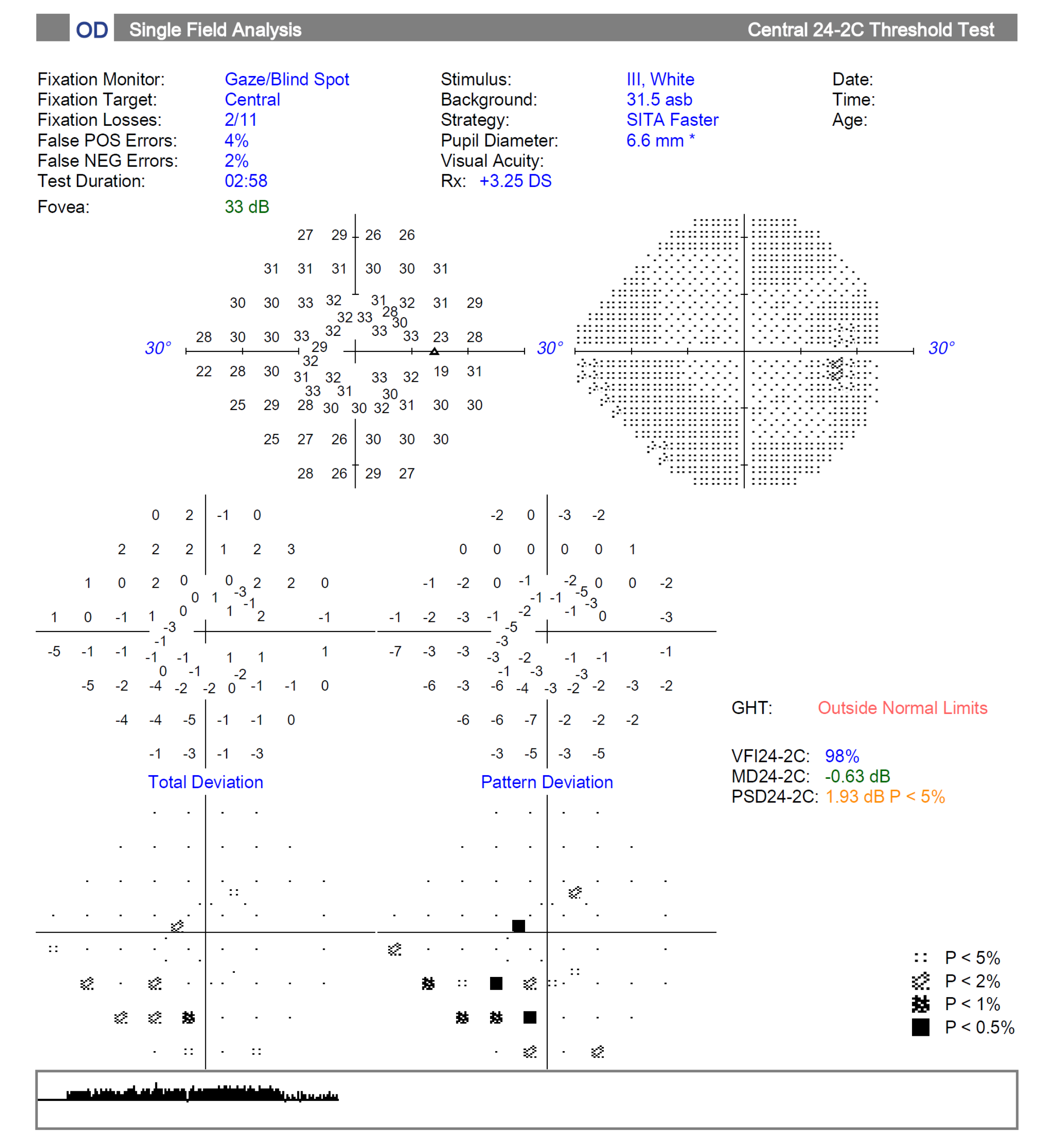
Figure 6 a – R VF 2022
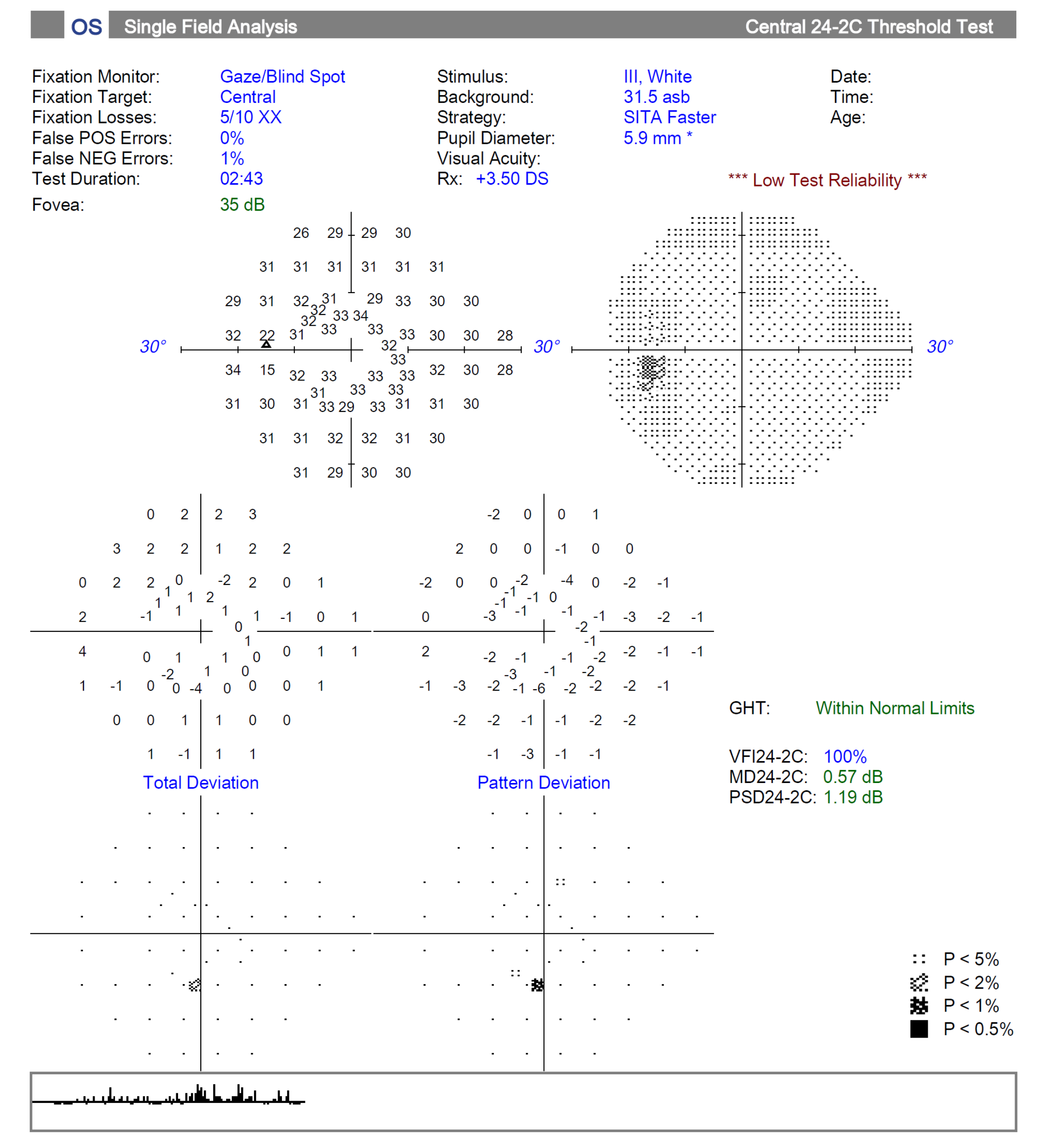
Figure 6b – L VF 2022
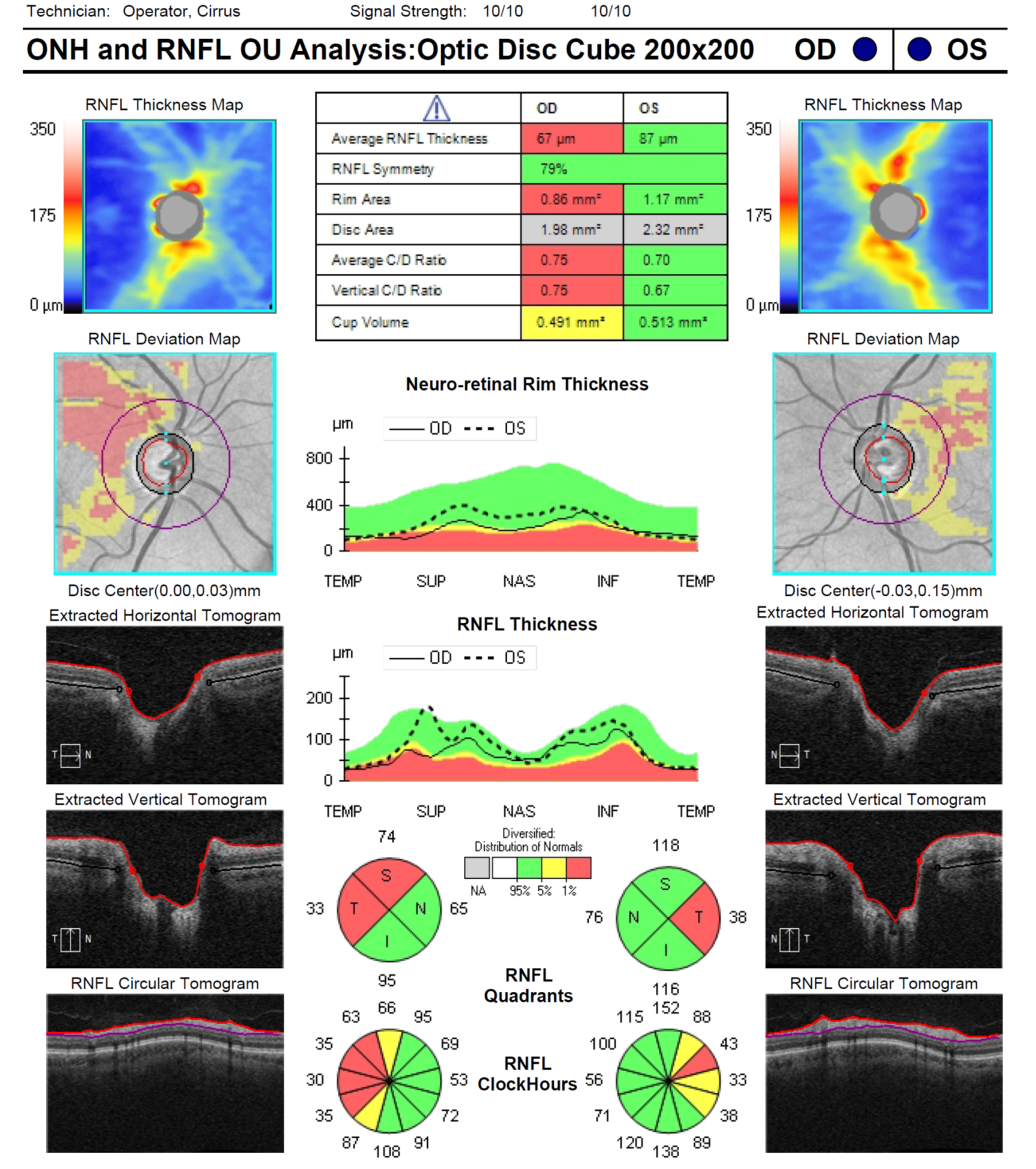
Figure 7 – RNFL OU 2022
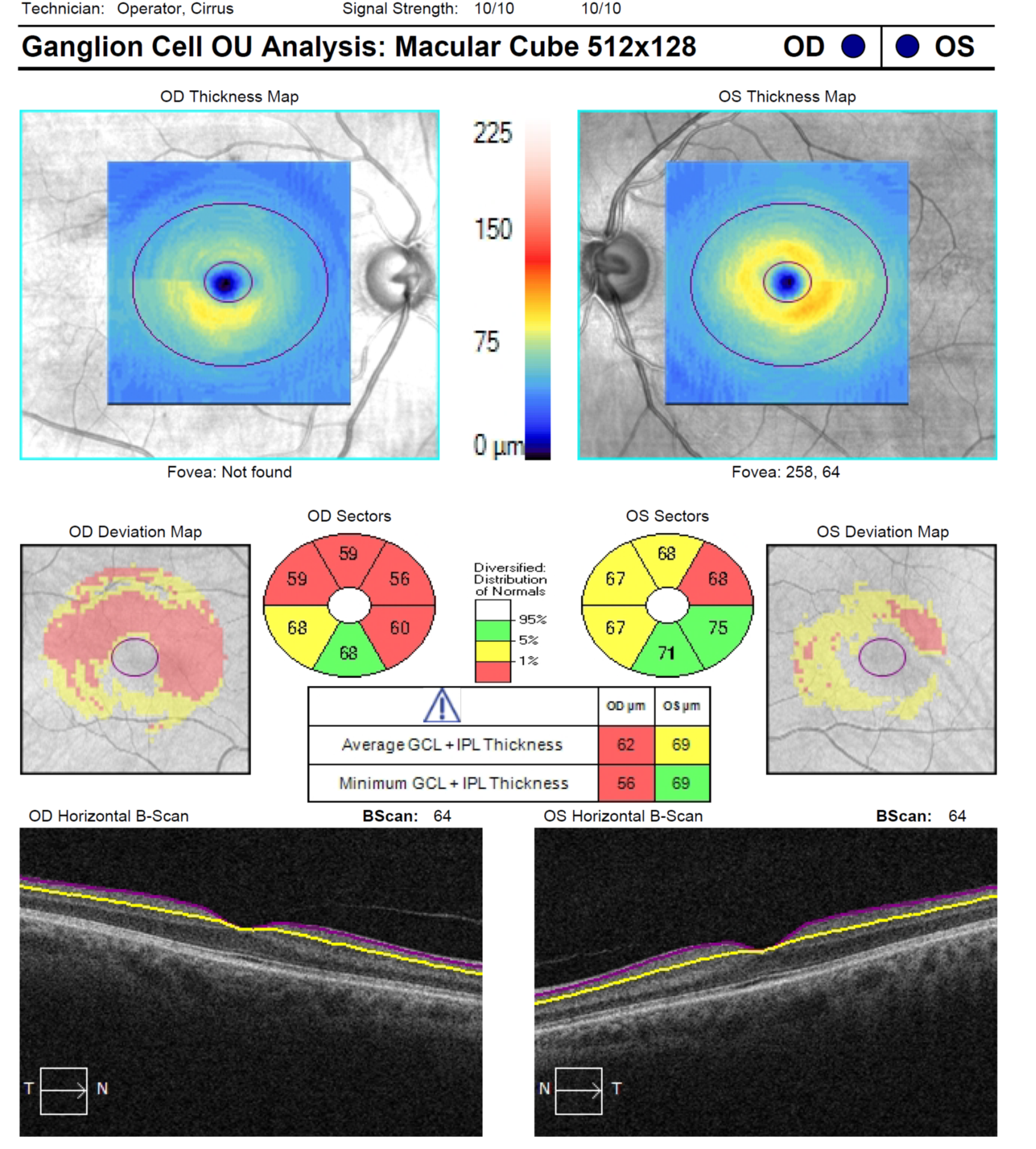
Figure 8 – GCC OU 2022