Case 4 – 2023
Learning outcomes:
- To understand the challenges of OCT assessment in patients with myopic optic nerves
- To be familiar with IOP-independent risk factors for glaucoma
- To determine when neuro-imaging is required in a patient with suspected NTG
- To consider tension series and the water drinking test in the assessment of patients with suspected undiagnosed IOP spikes
- To have a basic understanding of the genetics of glaucoma
A 70 year old female presents to you for a glaucoma assessment.
- Past ocular history: Moderate myopia and astigmatism
- Past medical history: Asthma, Migraines – less frequently post-menopause, Raynaud’s phenomenon
- Medications: Aspirin, Ventolin Inhaler
- Family history: Mother had glaucoma, diagnosed aged in her 60s, took eye drops
Examination
| Right eye | Left eye | |
| BCVA | 6/6 | 6/6 |
| IOP | 17 mmHg | 14 mmHg |
| Ishihara colour plates | 14/14 | 14/14 |
| Pupils | No RAPD | |
| Gonioscopy | D30r | D30r |
| Corneal Pachymetry | 501 µm | 503 µm |
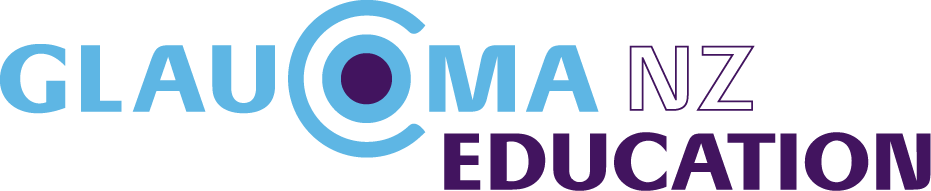
| Fundus examination | See optic nerve photo (Figure 1a). Macula clear. Peripheral retina clear and flat | See optic nerve photo (Figure 1b). Macula clear. Peripheral retina clear and flat |
| Visual Fields | See visual fields (Figures 2a and 2b) | |
| OCT | See RNFL analysis (Figure 3) and GCC scan (Figure 4) | |
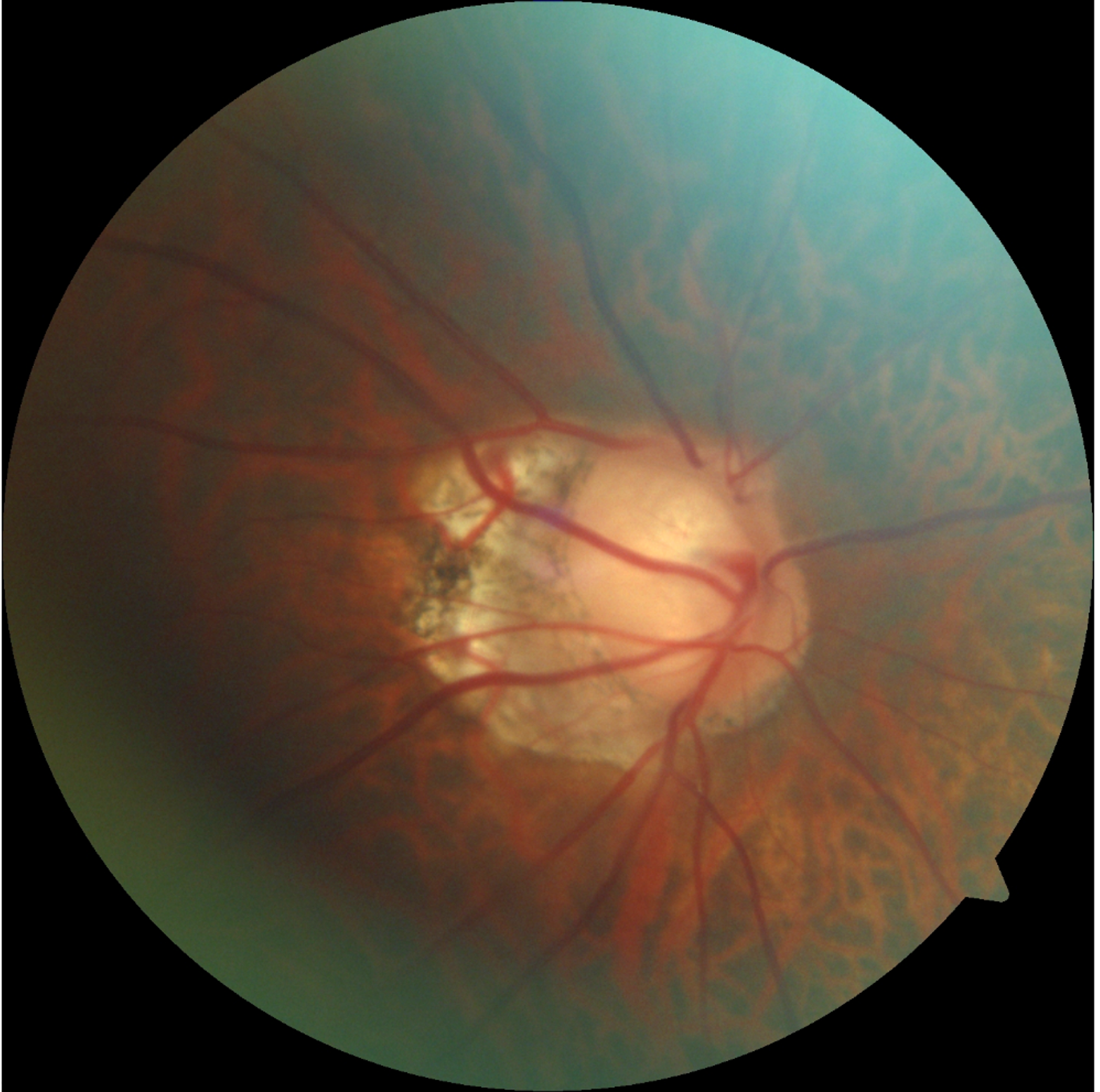
Figure 1 a – Right Optic Disc
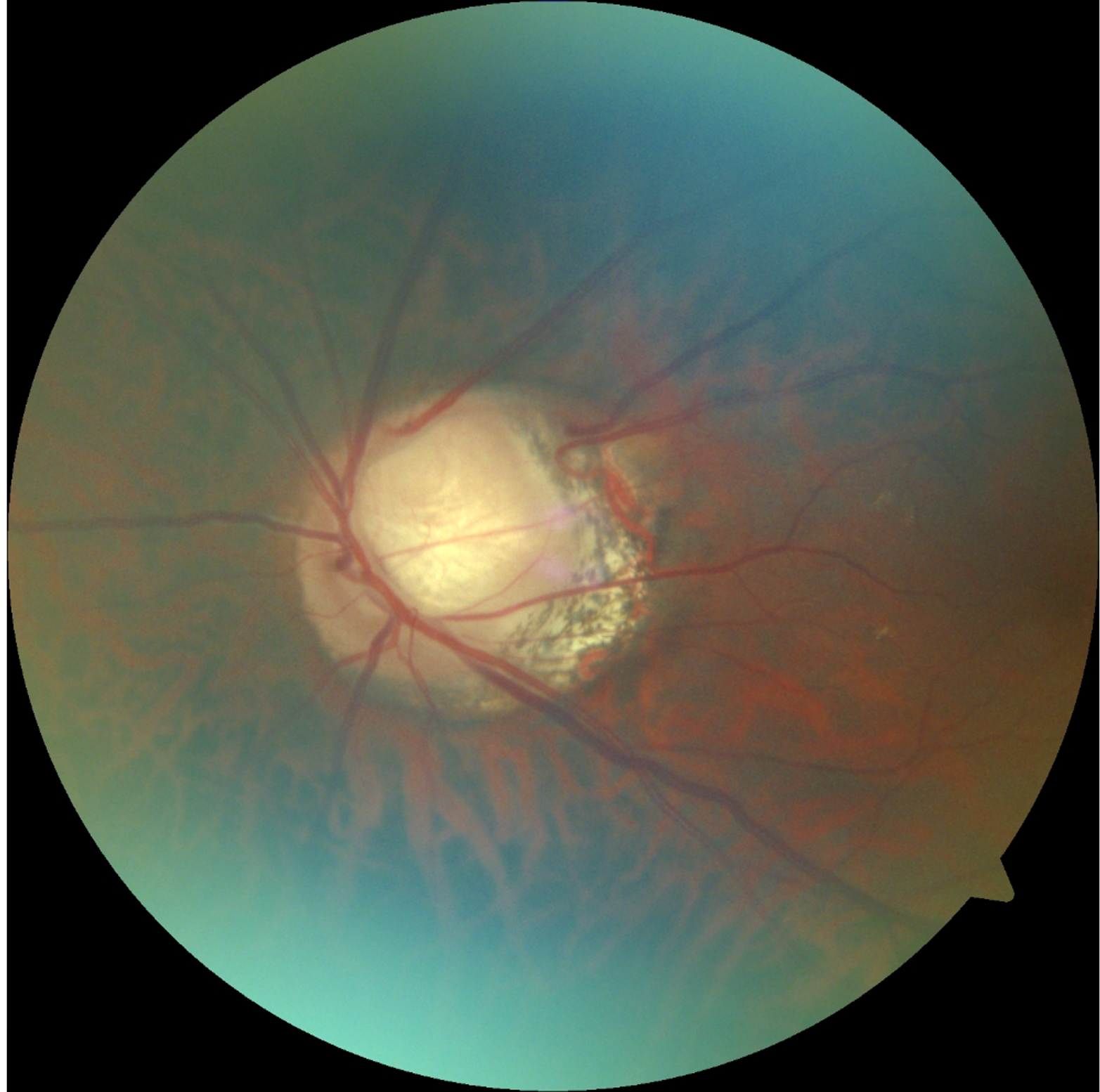
Figure 1 b – Left optic disc
Figure 2a – Right Visual Field
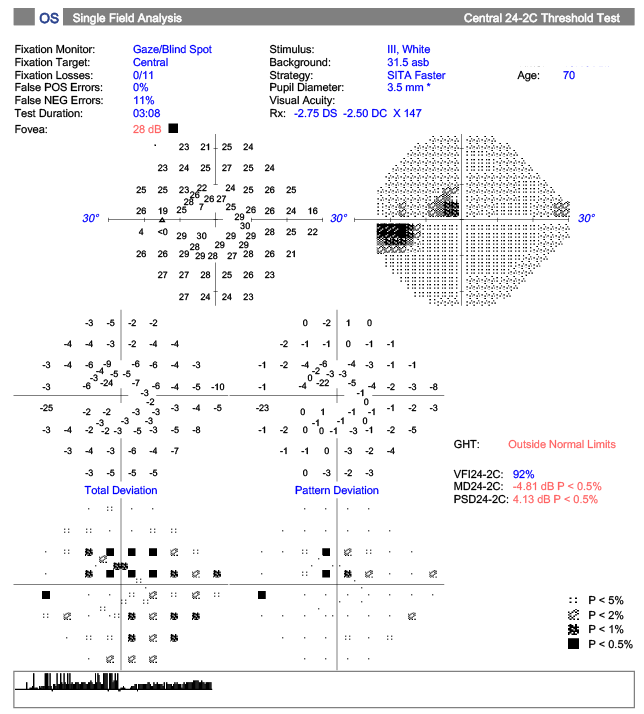
Figure 2b – Left visual field
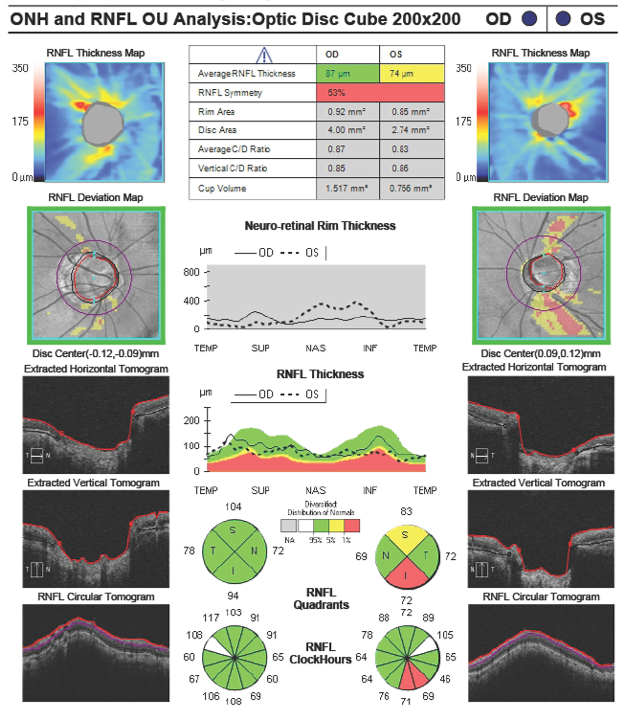
Figure 3 – RNFL OCT analysis both eyes
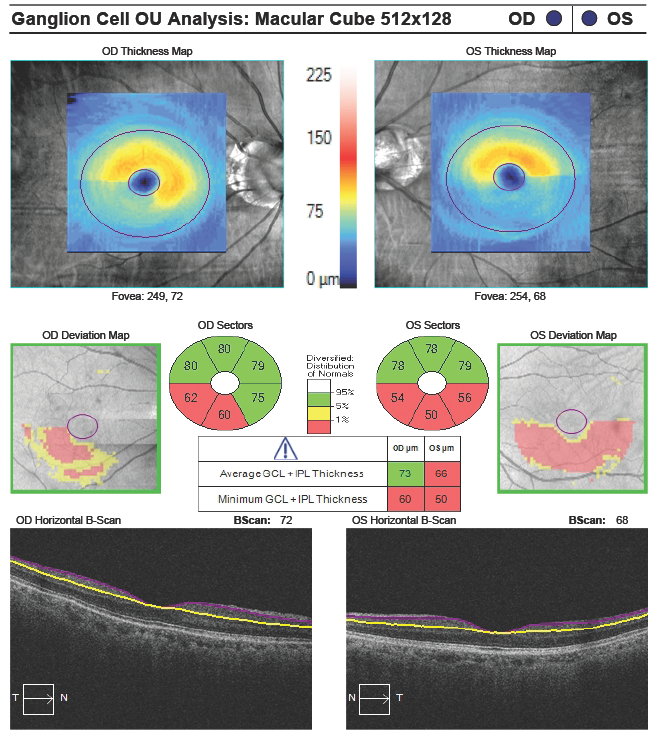
Figure 4 GCC OCT both eyes