Case 1 – 2024
Learning Outcomes
- Demonstrate an understanding of the differences between pigment dispersion syndrome, pigmentary ocular hypertension, and pigmentary glaucoma
- Analyse, interpret and correlate the findings with the diagnosis of pigmentary glaucoma
- Discuss treatment options and different treatment modalities for pigmentary glaucoma
Case history
A 68 year-old Caucasian male presents to your practice for a glaucoma assessment. He mentions having used eye drops in the past. He cannot remember their name but stopped 1-2 years ago. He also mentions undergoing some kind of laser treatment to the eyes but cannot remember why. He still wears glasses but usually removes them for reading. He has good general health and is not taking any medications. His family history includes glaucoma in his mother, diagnosed around age 70 and currently uses eye drops.
Your examination findings on presentation shown below.
Table 1: Clinical examination findings
| Right eye | Left eye | |
| Best corrected visual acuity | 6/6 | 6/7.5 |
| Subjective refraction | -3.00/-1.50 x 156 | -3.75/-0.50 x 012 |
| Intraocular pressure
Goldmanns |
28 mmHg |
30 mmHg |
| Perkins Pachymetry | 537 µm | 541 µm |
| Ishihara | 14/14 plates | 14/14 plates |
| Pupils | Small L RAPD | |
| Slit lamp examination
(See Figures 1 and 2) |
Corneal endothelial pigment and spoke-like mid-peripheral iris transillumination defects on retroillumination
Patent peripheral iridotomy at 12 o’clock |
Corneal endothelial pigment and spoke-like mid-peripheral iris transillumination defects on retroillumination
Patent peripheral iridotomy at 12 o’clock |
Figure 1: Composite image of anterior segment
Composite image of the anterior segment clinical findings. (Reproduced from Bustamante-Arias et al 2021)

Figure 2: Colour photos of right and left optic nerve heads
Right eye

Left eye

Figure 3: Visual field images
Right eye
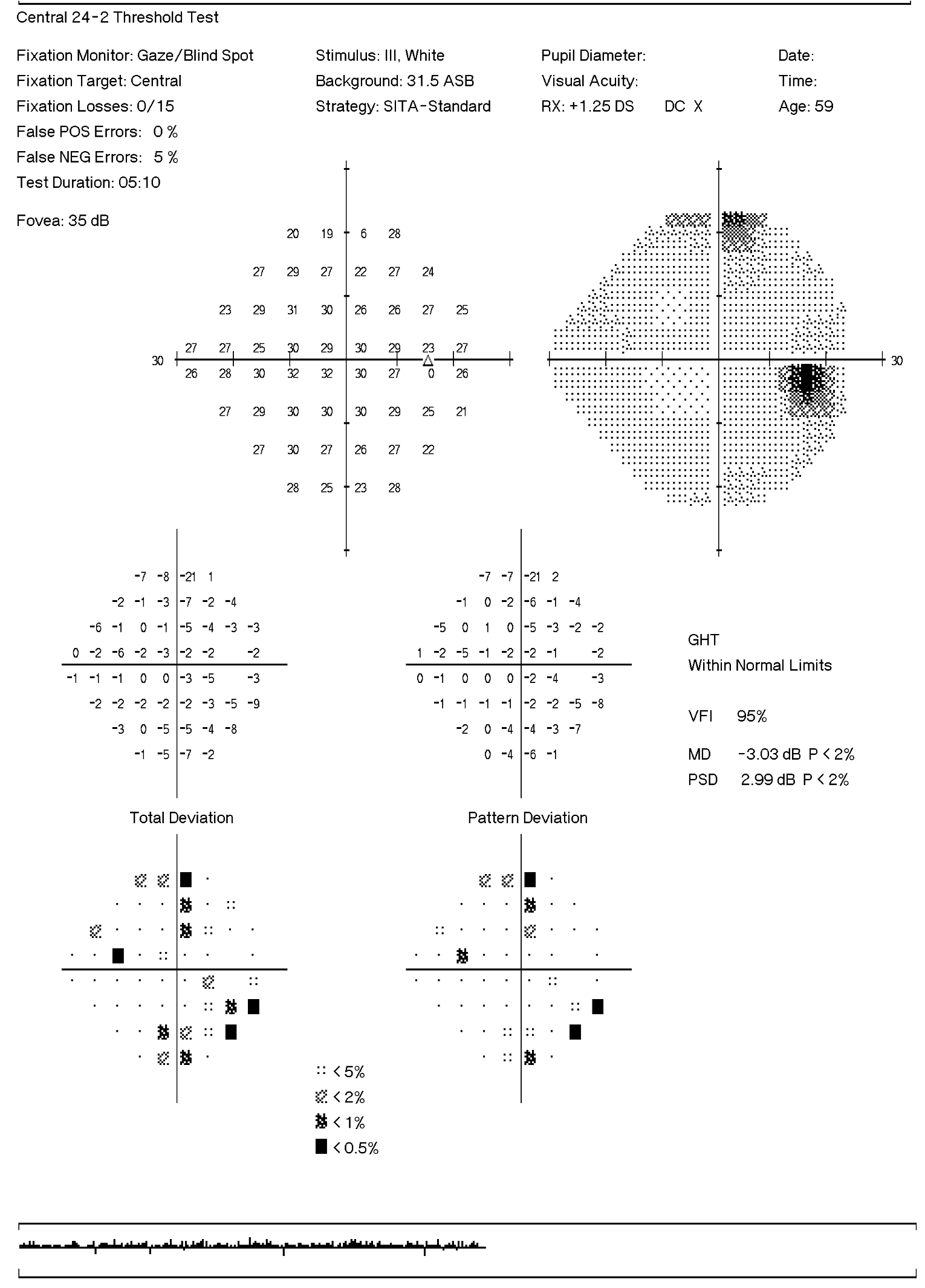
Left eye
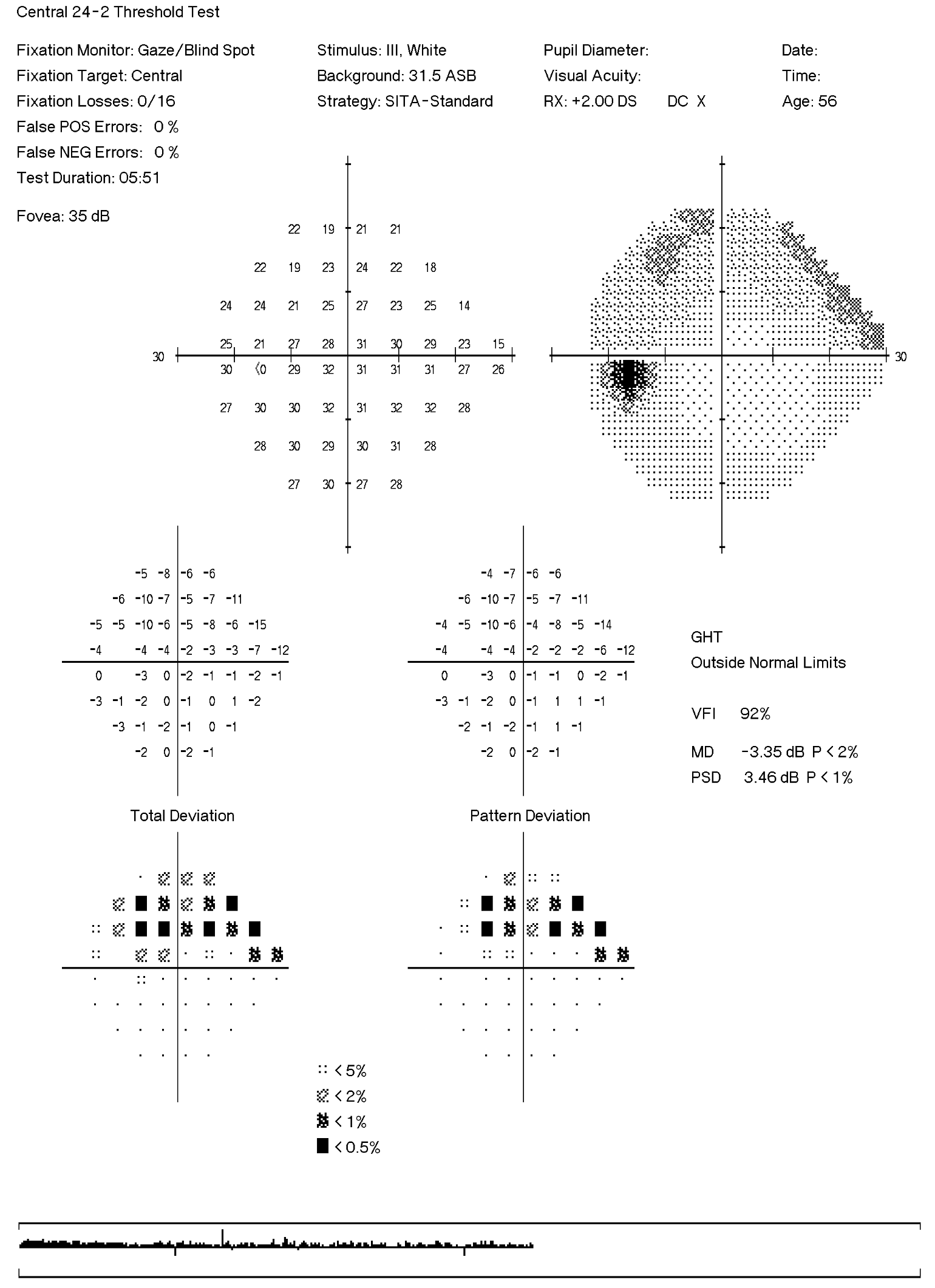
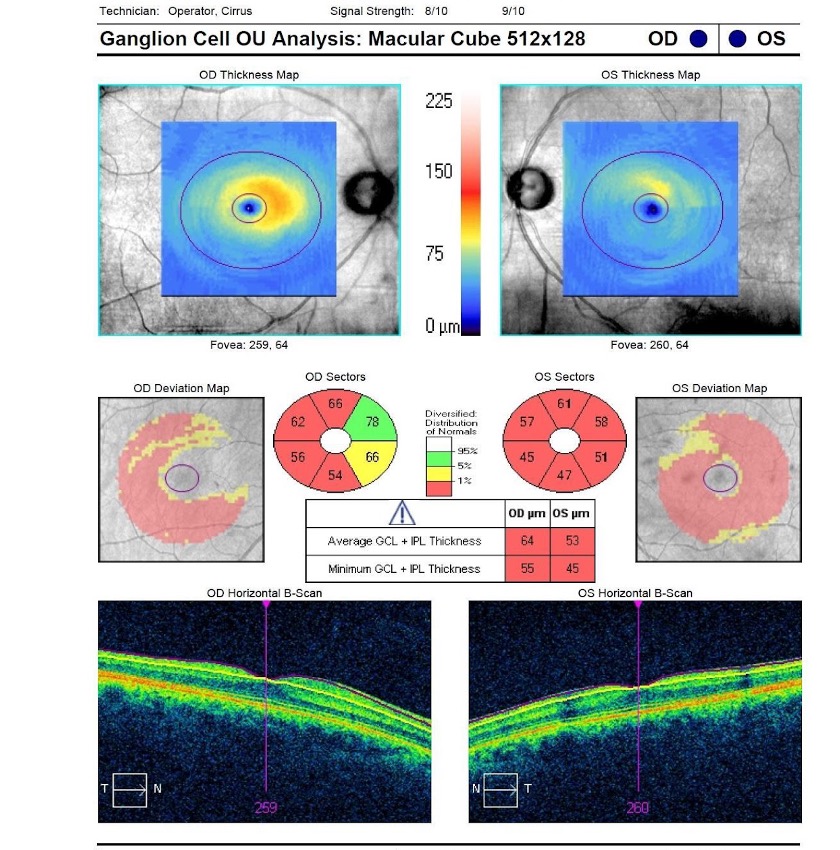
Figure 4: Retinal nerve fibre layer OCT scan analysis both eyes
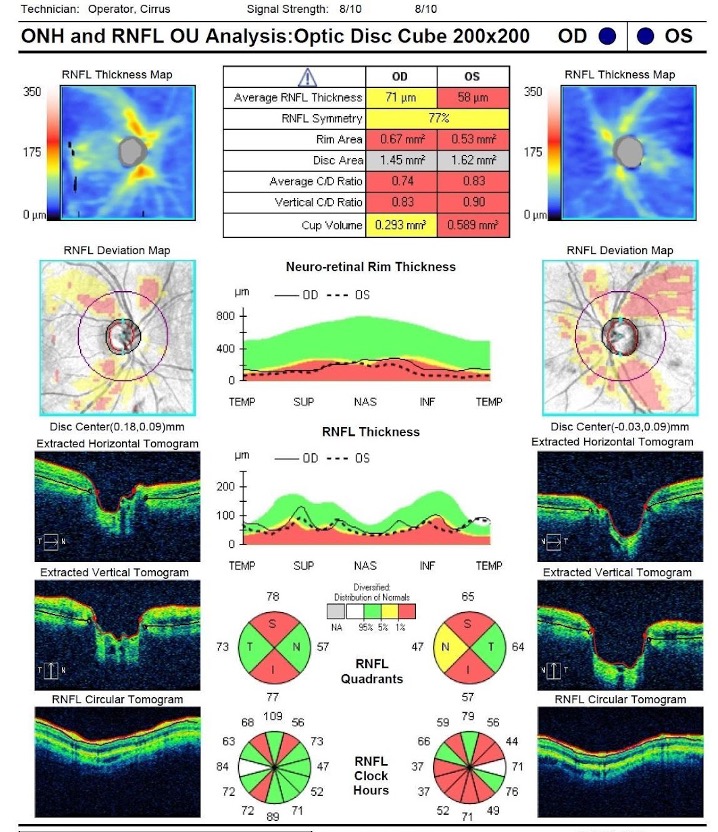
OCT macular scan ganglion cell complex both eyes