Case 4 – 2024
Learning Outcomes
- To understand the definition and pathophysiology of non-arteritic anterior ischaemic optic neuropathy (NAION)
- To recognise the clinical presentation of NAION
- To identify the risk factors associated with NAION
- To understand the management options for NAION
A 49 year-old Caucasian male presents to your practice reporting a 3 week history of right eye reduced vision. He tells you that he woke up 3 weeks ago with blurred vision in his right eye and is worried because it has not improved. He has no other ocular complaints. He denies any eye pain, redness, or discharge. He also denies any headaches, scalp tenderness, or pain on chewing. He has no recent unexplained weight loss.
Previous ocular history: Left eye patching as a child
Previous medical history: High cholesterol, borderline hypertension, concussion in 2011
Current medications: Statin, Fluoxetine
Family history: Nil
Smoking history: Ex-smoker
Examination
Examination findings on presentation shown below.
| Right eye | Left eye | |
| Best corrected visual acuity | 6/24 | 6/7.5-2 |
| Subjective refraction | +0.75 / -0.50 x 24 | +0.75 / -0.75 x 173 |
| Goldmann tonometry | 15 mmHg | 14 mmHg |
| Gonioscopy | Open | Open |
| Pachymetry | 586 µm | 597 µm |
| Extraocular eye movements | Full range
No pain, no diplopia |
Full range
No pain, no diplopia |
| Ishihara | 12/14 (Slow) | 14 / 14 |
| Pupils | R RAPD | |
| Anterior segment | Early lens opacification, otherwise unremarkable | Early lens opacification, otherwise unremarkable |
| Fundus examination | Swollen optic nerve
Macular clear Peripheral retina clear and flat |
Small congenitally anomalous optic disc
No haemorrhages Macular clear Peripheral retina clear and flat |
| Visual fields | See visual fields (Figure 1) | |
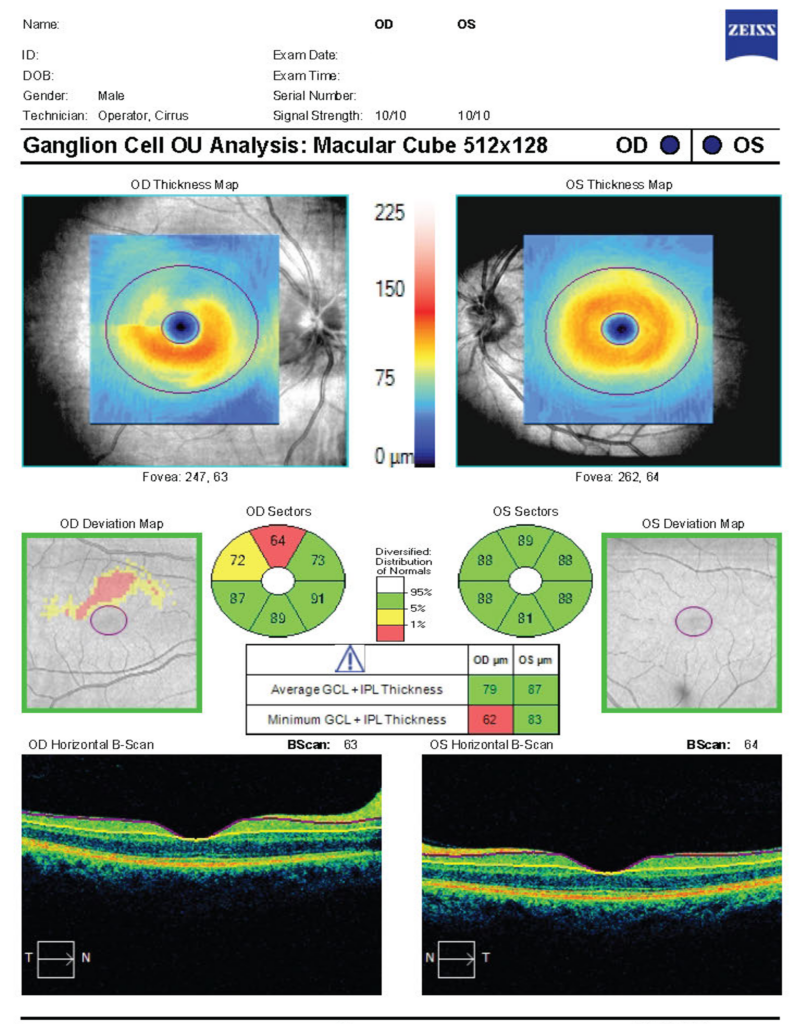
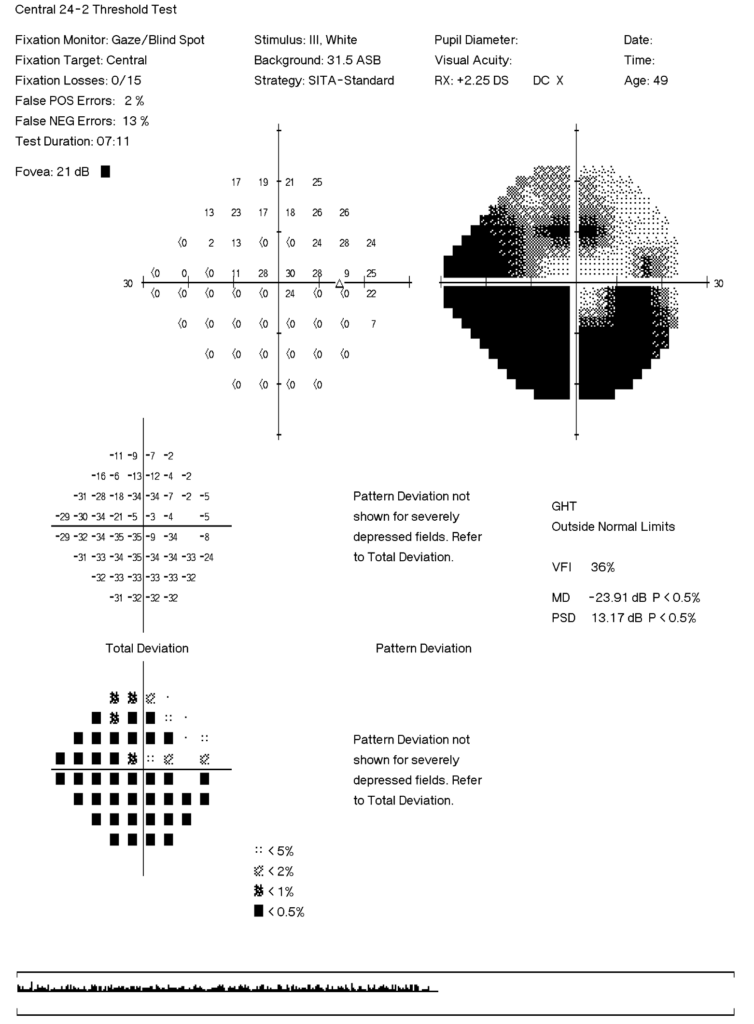
| OCT | See RNFL analysis (Figure 2) and GCC scan (Figure 3) | |
Figure 1: Visual fields
Right eye

Left eye

Figure 2: RNFL thickness analysis
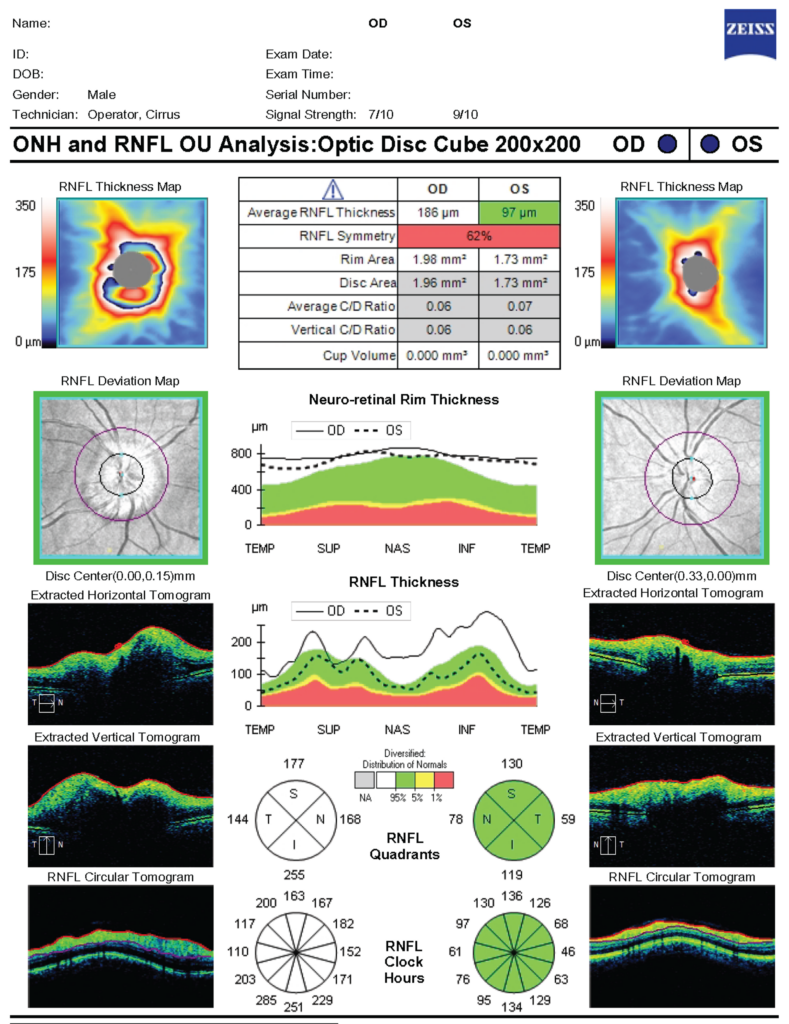
Figure 3: GCC thickness analysis
The patient returns 2 months later for his follow up appointment. Examination findings from that appointment are shown below.
| Right eye | Left eye | |
| Best corrected visual acuity | 6/19 | 6/9.5-1 |
| Goldmann tonometry | 16 mmHg | 14 mmHg |
| Gonioscopy | Open | Open |
| Pachymetry | 586 µm | 597 µm |
| Extraocular eye movements | Full range
No pain, no diplopia |
Full range
No pain, no diplopia |
| Ishihara | 14/14 | 14 / 14 |
| Pupils | R RAPD | |
| Anterior segment | Early lens opacification, otherwise unremarkable | Early lens opacification, otherwise unremarkable |
| Fundus examination | See disc photos (Figure 4)
Macular clear Peripheral retina clear and flat |
See disc photos (Figure 4)
Macular clear Peripheral retina clear and flat |
| Visual fields | See visual fields (Figure 5) | |
| OCT | See RNFL analysis (Figure 6) and GCC scan (Figure 7) | |
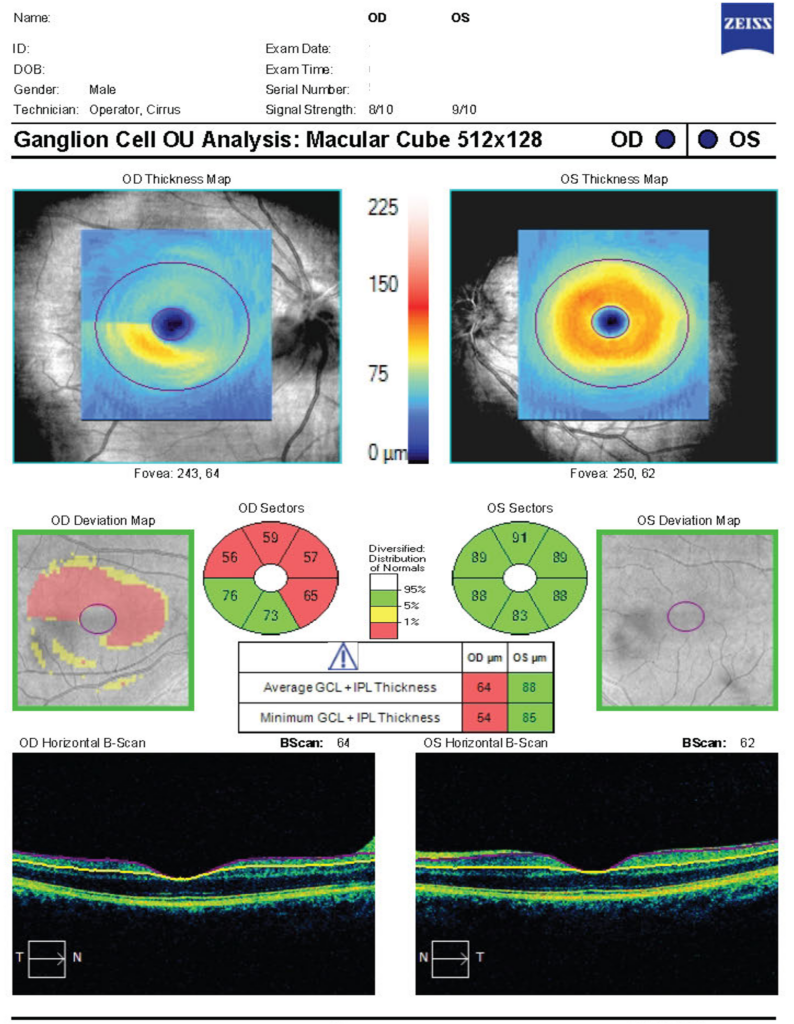
Figure 4: Colour photos
Right eye
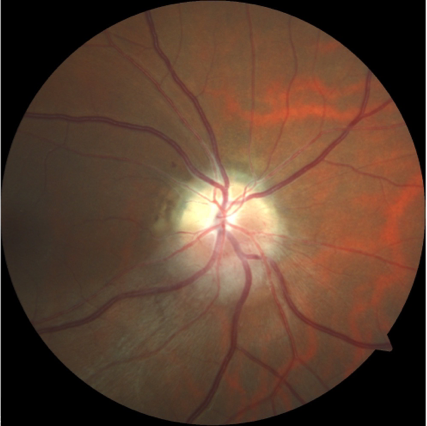
Left eye
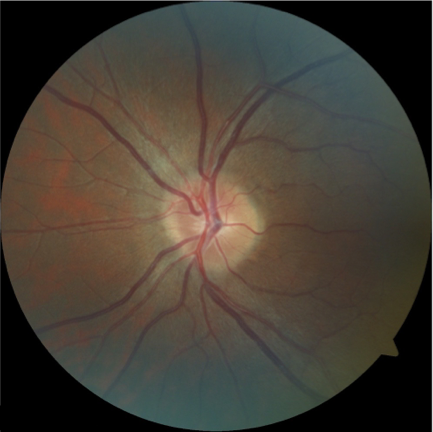
Figure 5: Visual fields – 2 months
Right eye
Left eye

Figure 6: RNFL thickness analysis – 2 months

Figure 7: GCL thickness analysis – 2 months
Long-term retinal nerve fiber layer changes following nonarteritic anterior ischemic optic neuropathy
Current concepts in the diagnosis, pathogenesis and management of nonarteritic anterior ischaemic optic neuropathy
The fellow eye in NAION- report from the ischemic optic neuropathy decompression trial follow-up study
Retinal Ganglion Cell Layer Thinning Within One Month of Presentation for Non-Arteritic Anterior Ischemic Optic Neuropathy
NAION or not NAION_ A literature review of pathogenesis and differential diagnosis of anterior ischaemic optic neuropathies